Past Issues
Evaluate The Retention of Conventional Cast Gold Post-And-Cores Compared to CAD/CAM Fabricated Printed, Milled Titanium Post-And-Core and Milled Zirconia Post-and-Cores Based on Load–An Invitro Study
Yesh Sharma*
Assistant Professor, Department of Conservative Dentistry and Endododntics, Pacific Dental College and Hospital, Udaipur, India
*Corresponding author: Dr. Yesh Sharma, Assistant Professor, Department of Conservative Dentistry and Endododntics, Pacific Dental College and Hospital, Udaipur, India, Tel: 7353693127; E-mail: [email protected]
Received Date: April 29, 2024
Publication Date: September 23, 2024
Citation: Sharma Y. (2024). Evaluate The Retention of Conventional Cast Gold Post-And-Cores Compared to CAD/CAM Fabricated Printed, Milled Titanium Post-And-Core and Milled Zirconia Post-and-Cores Based on Load–An Invitro Study. Dental. 6(2):14.
Copyright: Sharma Y. © (2024).
ABSTRACT
Aim: Computer-aided design/computer-aided manufacturing (CAD/CAM) technology is gaining popularity in dentistry, and more recently, used to fabricate custom post-and cores (PC) for endodontically treated teeth. The purpose of this study was to evaluate the overall retention of conventional cast gold post-and-cores compared to CAD/CAM fabricated printed, milled titanium post-and-core and milled zirconia post-and-cores based on load, time of dislodgement. Results: Pull out test revealed higher retention values for (CPTPC) and (CMTPC) among the groups. When compared to (CMZPC), conventional (CCGPC) revealed significantly better retention values. Cohesive failure was observed with groups I, II and IV. However, group III revealed a mixed type of failure.
INTRODUCTION
Cast post-and-core (CPC) is commonly used to restore endodontically treated teeth with extensive coronal structural loss. Retention of CPC is a fundamental factor influencing definitive restoration longevity and success. Length, shape, diameter, and post surface, as well as the type of cement used, are associated factors that may affect CPC retention and stability [1]. Custom CPC is documented to have superior adaptation and fit to the radicular post space walls when compared to prefabricated post [2].
Moreover, gold alloy creates a layer of chromium oxide that resists tarnish. Custom-made PC has been reported with some disadvantages, for example, most abutments break at a point beyond the half distance of the root length due to its high stiffness. If these teeth abutments fracture, usually they are unrestorable [3]. Custom-made PC has also been reported to be fabricated out of zirconia to overcome esthetic limitation associated with metal CPC.
This has been made possible due to the following properties of zirconia; high flexural strength, high fracture toughness, chemical stability, biocompatibility, favourable optical properties, greater toughness and maximum adaptability to the canal and appropriate esthetic characteristics.
However, the use of zirconia PC to restore endodontically treated teeth has limitations. In relation to its rigidity, zirconia posts cause more catastrophic root fractures than fiber posts. Also, the surface of zirconia posts does not bond to resin composite materials, leading to an inferior post retention [4]. Another limitation of zirconia PC is the difficulty in retrievability when endodontic retreatment is required.
Titanium has gained wide acceptance in dentistry due to its biocompatibility, excellent corrosion resistance, reduced cost, ease of fabrication (milling) and high mechanical properties. Titanium can be found in different combinations for use in dentistry [5]. Pure titanium is composed by 99.5 % titanium and 0.5 % of interstitial elements (carbon, oxygen, nitrogen, hydrogen and iron) and the proportion of these elements directly affects the metallic properties.
The ASTM (American Society of Testing and Materials) the standard of F1295 specifies titanium in different grades according to its purity, which is evaluated according to the amount of oxygen. The titanium melted only from titanium sponge is known as titanium grade 1, which is considered the most-pure grade. When titanium sponge is mixed with titanium fragments, the amount of oxygen (O2) and iron (Fe) increase and titanium becomes harder. The more fragments are added, the harder the titanium becomes (titanium grades 2, 3 and 4) [6,7].
To the best of our knowledge, there are no in-vitro studies assessing the relationship of the retention of custom cast post-and-core (Gold) and, custom milled post-and-core (Titanium) alloy, custom printed post-and-core (Titanium) alloy and custom milled post-and-core (Zirconia) [8].
The aim of this study was to evaluate the difference in the retention between custom cast post-and-core (Gold), custom printed post-and-core (Titanium) alloy, custom milled post-and-core (Zirconia) and custom milled post-and-core (Titanium) alloy [9,10].
MATERIALS AND METHODS
Eighty sound maxillary central incisors extracted for periodontal reasons were selected. Exclusion criteria included presence of caries, restoration, root canal treatment (RCT), crack/s, attrition, very long or very short teeth, and/or severe root curve. Teeth were thoroughly cleaned with a brush after the extraction and a sharp scalpel was used to remove any soft tissue from the root surfaces. Any remaining tissues were carefully removed by using a periodontal curette. Teeth were subsequently stored in 0.2 % sodium aide for at least 24 hours prior to the specimen’s preparation (ISO 28399, 2011).
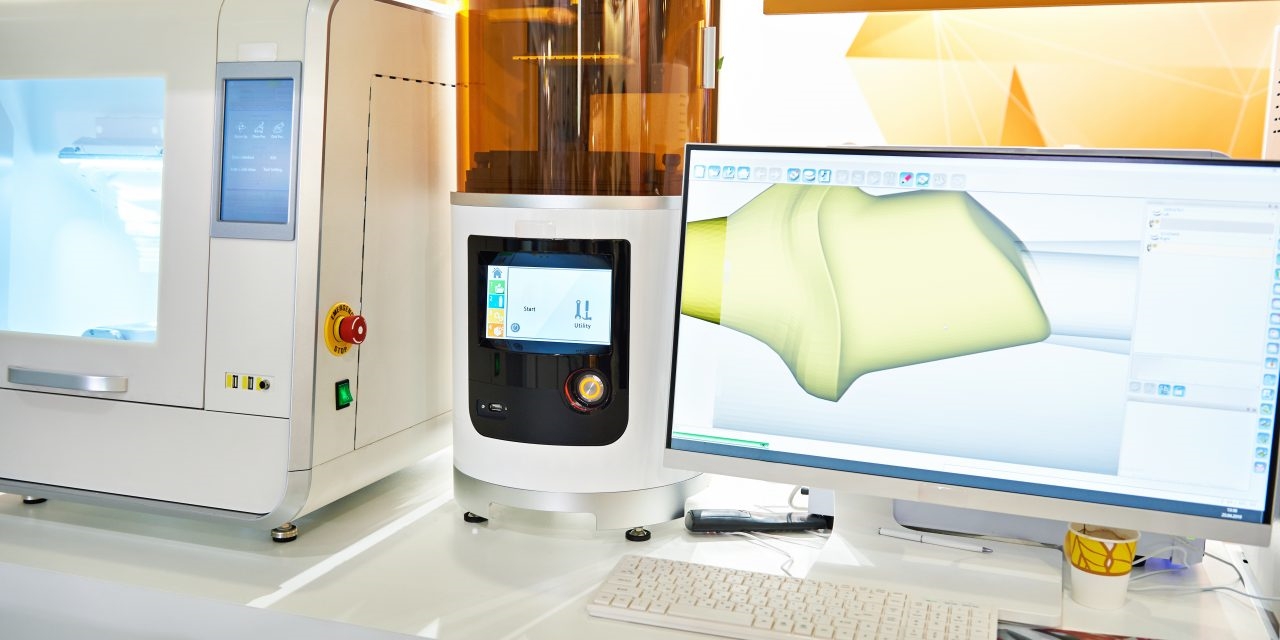
Figure 1. Computer-aided design/computer-aided manufacturing (CAD/CAM)
Each tooth was randomly assigned by a number (from 1 to 40). Then the teeth were randomly allocated into four groups (n=10 each), group A was restored with custom cast post-and-core (Gold) and group B was restored with custom milled post-and-core (Titanium) alloy, group C was restored with custom printed post-and-core (Titanium) alloy and group D was restored with custom milled post-and-core (Zirconia). Each root length was measured from apex to the labial middle point of the cemento-enamal junction, together with labiolingual and mesiodistal dimensions at the level of the cervical margin with a digital caliper (Links Brand; Harbin Metering Instrument Works, Harbin, China). These measurements were recorded, and the average values calculated for statistical analysis.
The specimens were individually embedded (mounted) in special specimen holder by means of epoxy resin (Exakto-form, Bredent) with elasticity modulus of 12 GPa. which is similar to elastic modulus of human bone (18 GPa) with the use of a test mount former, 2cm in dimension, 2-3 mm below the cemento-enamel junction (CEJ). A prefabricated printed jig made from Form labs printer (Somerville, Massachusetts, United states) was used to position each tooth test mount former during immersion of the teeth in acrylic resin to standardize teeth position to be centralized within the test mounts.
Figure 2. Cast Post-And-Core (CPC).
The mount test jig was used to standardize the teeth position while performing teeth preparation and RCTs. During the polymerization of the acrylic resin, the acrylic resin block was cooled in water to avoid dehydration of the teeth. The teeth were prepared to have 2 mm ferrule and a 1mm shoulder finish line.
Preparation of the access cavity was done using a size 2 diamond round bur mounted to a high-speed handpiece. The working length was established 1 mm shorter than the root apex. Root canal preparation for each tooth was performed up to file size 40 (Kerr/Sybron Corp). Flaring the coronal part of each root canal was performed using Gates Glidden burs number 2-4. Each root canal was irrigated with NaOCl 2.5% and EDTA 18% (chelating agent) (Ultradent Products, Inc) to remove the smear layers. Following irrigation, prepared root canals were dried with sterile paper points (Sureendo, Gyeonngi-do, South Korea) before obturation. A size 40 gutta-percha master cone (Dentsply Maillefer) coated with AH Plus sealer (Dentsply DeTrey, Kontanz, Germany) was inserted into the canal. Root canals were obturated using lateral condensation technique with finger spreaders (Dentsply Maillefer). Finally, excess gutta-percha (Dentsply Maillefer) was removed and the remaining was condensed with a hot plugger.
Definitive post length was prepared and established with the use of peeso reamers (Maillefer S.A., Ballaigues, Switzer- land) up to size 3. To obtain a standardized length for the posts, the coronal portion of the gutta percha was removed with hot plugger until adequate length (11mm) was achieved. Each root canal was cleaned by using air/water spray, EDTA and then dried by paper points.
40 custom post-and-cores were fabricated with the use of auto polymerizing acrylic resin (Pattern Resin LS; GC) and serrated plastic post (M). Serrated plastic post was relined with acrylic resin then inserted in the root canal. Then the core was built up using GC pattern, and prepared using a diamond bur (diamond bur of head size ISO No. 010. to achieve a core with 4 mm height. A plastic loop was attached to the coronal part of the GC pattern core which was used to be attached to the Instron machine (Instron Corp, Norwood, MA) during the pull out test.
Each post was randomly divided in to four groups as shown. Twenty acrylic resin pattern posts were cast with a Type IV gold alloy using the conventional lost wax casting technique. Sixty acrylic resin pattern posts were scanned in a desktop scanner (3Shape D900L, 3Shape Dental System). STL files for each scanned post-and-core as shown was sent to Core 3D and Renovis for the fabrication of 10 milled titanium, 10 printed titanium and 10 milled zirconia post-and-cores each. The prepared specimens were stored in 100% humidity at room temperature to simulate the humidity in vivo until they were returned for testing.
According to the manufacture recommendation, group 1 CPC gold, group 2 CPPC titanium, group 4 CMPC titanium were treated first using ultrasonic cleaning solution in 96% isopropyl (3 minutes) and then airborne-particle abraded (50 μm Al2o3 at 2.8 bar for 5 second). Group 3 CMPC zirconia was treated using ultrasonic cleaning in 96% isopropyl (3 minutes), Rocatec soft (30 μm airborne-particle abrasion at 2.8 bar for 12 second over entire zirconia surface and then, silane coupling agent (Espe-Sil) applied.
The post-and-cores for all samples were coated with Rely X Unicem resin cement (3M ESPE, Seefeld, Germany) and mixed according to manufacturer’s instructions (3M ESPE). Also, cement was applied into the root canals by using Elongation tip to the nozzle (3M ESPE). After that posts were inserted gently into the root canals to reduce hydrostatic pressure, they were positioned in place under firm finger pressure and the excess cement was removed. Then specimens of each group (n=10) were kept in normal saline for 24 hours in a refrigerator before testing.
Each tooth was subjected to a pull out test with a universal Instron Testing Machine (Instron Corp, Norwood, MA) at a crosshead speed of 0.5mm/min. The device was calibrated before placing each sample. The position and the direction of the samples in the machine were set by the device itself. The specimens were placed in a customized, self- aligning apparatus to standardize the position and the direction of the samples in the machine. The horizontal rod attached to the upper element of the Instron testing machine (ITM) was passed through the hole which was made in the CPC as hook attachment.
RESULTS
The difference in retention for the different types of post-and-cores was evaluated. The mean and median values of retention for groups were calculated. By using Mann-Whitney U test with Bonferroni adjustment to compare median of total time, average load and displacement variables of each group with gold control group, it was determined that retention between the custom printed titanium post-and-core (CPTPC), custom milled titanium post-and-core (CMTPC), custom cast gold post-and-core (CCGPC) and custom milled zirconia post-and-core (CMZPC) was significant.
DISCUSSION
Several studies have reported acceptable clinical outcomes with custom cast gold post-and-cores and hence they are considered to be the ‘gold standard’ and was used as a control group in this study. However, there is lack of strong evidence that printed/milled titanium technique post-and-core provides comparable retention and effectiveness. Many investigators have reported that the material and design of cast post-and core affect the success of endodontically treated teeth restored with post-and-cores. The custom cast gold post-and-core as mentioned has been regarded as the gold standard for foundation restoration due to its high biocompatibility, corrosion resistance and high rigidity and has been used extensively.
Creugers et al. reviewed the literature and reported that the success and survival rates have varied in endodontically treated teeth restored with different post-and-core systems. No consensus exists on which technique and materials are best suited for use. Recently, Wei Liu et al. found that post-and cores fabricated by CAD-CAM milled technique using cobalt-chromium alloy could be an alternative to conventional casting for metal post-and-core fabrication. However, the retention of CAD-CAM milled or printed post-and-cores was not evaluated and tested in this study.
CONCLUSION
Within the limitations of the present study and based on the findings, the use of custom printed and milled titanium post-and-cores showed comparable results when compare to custom cast gold post-and-core. Custom milled zirconia post-and-cores revealed significantly lower retention compared to other groups. The use of titanium alloy fabrication of post-and-core is effective in retention and could be an alternative material of choice to gold alloy. Among 4 groups, the custom milled zirconia post-and-core showed least bond to resin cement materials, leading to significantly lower post retention. Further studies with in-vivo testing is required to confirm the conclusions from this study.
REFERENCES
- Fernandes AS, Shetty S, Coutinho I. (2003). Factors determining post selection: a literature review. J Prosthet Dent. 90(6):556-562.
- Bergman B, Lundquist P, Sjögren U, Sundquist G. (1989). Restorative and endodontic results after treatment with cast posts and cores. J Prosthet Dent. 61(1):10-15.
- Creugers NH, Mentink AG, Käyser AF. (1993). An analysis of durability data on post and core restorations. J Dent. 21(5):281-284.
- Pontius O, Nathanson D, Giordano R, Schilder H, Hutter JW. (2002). Survival rate and fracture strength of incisors restored with different post and core systems and endodontically treated incisors without coronoradicular reinforcement. J Endod. 28(10):710-715.
- Balkenhol M, Wöstmann B, Rein C, Ferger P. (2007). Survival time of cast post and cores: a 10-year retrospective study. J Dent. 35(1):50-58.
- Heydecke G, Butz F, Hussein A, Strub JR. (2002). Fracture strength after dynamic loading of endodontically treated teeth restored with different post-and-core systems. J Prosthet Dent. 87(4):438-445.
- Awad MA, Marghalani TY. (2007). Fabrication of a custom-made ceramic post and core using CAD-CAM technology. J Prosthet Dent. 98(2):161-162.
- Lee JH, Sohn DS, Lee CH. (2014). Fabricating a fiber-reinforced post and zirconia core with CAD/CAM technology. J Prosthet Dent. 112(3):683-685.
- Baba NZ, Golden G, Goodacre CJ. (2009). Nonmetallic prefabricated dowels: a review of compositions, properties, laboratory, and clinical test results. J Prosthodont. 18(6):527-536.
- Ozkurt Z, Işeri U, Kazazoğlu E. (2010). Zirconia ceramic post systems: a literature review and a case report. Dent Mater J. 29(3):233-245.
 Abstract
Abstract  PDF
PDF