Past Issues
Demystifying the Depigmentation Manoeuvre: A Pragmatic Approach
Sumit munjal1*, Seema munjal2, Mohd rehan3, Sachin khurana4
1Dr Sumit Munjal, M.D.S., Professor, Department of Periodontics, Institute of Dental Studies & Technologies, UP, India 2Dr Seema Munjal, M.D.S., Reader, Department of Prosthodontics and crown & bridge, Ex- Dr. BR Ambedkar Institute of Dental Sciences & Hospital, Patna, Bihar, India 3Mohd Rehan, M.D.S., Reader, Department of Periodontics, Institute of Dental Studies & Technologies, UP, India 4Dr Sachin Khurana, M.D.S., Ex- Post graduate student, Department of Periodontics, Institute of Dental Studies & Technologies, UP, India
*Corresponding Author
Sumit Munjal, Department of Periodontics, Institute of Dental Studies & Technologies, UP, India, Tel: +91-9910259040; E-mail: [email protected] Received: December 02, 2020 Published: December 31, 2020
ABSTRACT
Gingiva participates in the harmony of smile with its pigmentation playing a crucial role. The condition is benign but is definitely unesthetic to patients. Depigmentation treatment is often sought for by today’s patient and numerous modalities are available for the same. The gingival biotype, clinician’s expertise, patient preferences, and recurrence rate, greatly determine the selection of a technique. We embraced the simple yet predictable surgical approach in the present article. Above all, the results were excellent as perceived by the patient.
Keywords: Gingival Depigmentation; Esthetics; Pigmentation; Articaine; Scalpel; Bur abrasion
INTRODUCTION
Esthetic is defined as “Appreciative of responsive to, what is pleasurable to the senses of beauty and culture”. Dental esthetics has become increasingly important in the practice of modern dentistry and is synonymous with a natural, harmonious appearance [1,2]. Gingiva participates in the harmony of smile with its pigmentation playing a crucial role. It is well documented in literature and etiology is multifactorial including genetic factors, tobacco use, systemic disorders and prolonged administration of certain drugs especially antimalarials and tricyclic antidepressants. Even though the condition is benign, yet pigmentation of gingiva is considered to be unesthetic by patients, and it may have a psychological impact on them [3]. The five primary causative pigments stated are melanin, melanoid, oxyhemoglobin, reduced hemoglobin, carotene; and others like bilirubin and iron [4].
Gingival depigmentation is a periodontal plastic surgical procedure [5] whereby hyperpigmentation is removed or reduced. The various techniques suggested in previous studies are: -
- Split thickness epithelial excision/scalpel surgical technique/surgical stripping [6]
- Gingival abrasion [7]
- Free gingival grafting [3]
- Electrosurgery [3]
- Cryosurgery [7]
- Radiosurgery [8]
- Soft tissue lasers [9]
- Acellular dermal matrix allograft [3]
- By Chemical methods: Using agents such as alcohols, phenols and ascorbic acid [3]
A simple expedient method is described in this article. Note worthily, the same did not require sophisticated instruments and apparatus. Nonetheless, it yields acceptable results thereby satisfying the patient’s concern.
CASE REPORT
A 22-year-old female reported to the Department of Periodontology and Implantology, with a chief complaint of blackish discoloration (Figure 1) of the front gum region. The patient observed the same for the past two years. On examination, lips were competent, with intraoral findings of melanin pigmentation seen at attached gingiva including papillae. The involvement was noted in both maxillary and mandibular anterior region from around premolar to premolar area, besides mild stains and calculus. Complete blood count (CBC) was done thereafter, in order to particularly evaluate the bleeding, clotting time, and haemoglobin percentage. All the values were found to be in the normal range. All the treatment modalities were explained and a duly signed written informed consent was obtained from the patient prior to the operative phase.
CLINICAL PROCEDURE
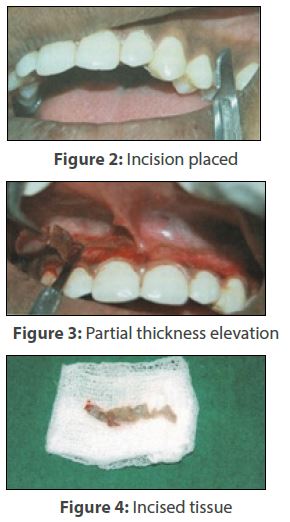
Following thorough oral prophylaxis, the site was anesthetized using 4% articaine HCl with 1:100,000 adrenaline by mucosal infiltration. Using a 15 no. Bard‑Parker blade and scalpel, two incisions were placed (Figure 2), which was held parallel to the gingival surface. These extended from gingival margin to the vestibular area, a little beyond the limits of the pigmented band. The vertical cuts demarcated the surgical area. Epithelium and a portion of the connective tissue was gingerly sliced in the partial thickness fashion (Figure 3) and dissected out (Figure 4) from one end of the vertical incision. The due significance was given to the physiological saline irrigation throughout whole process until completion.
Care was taken, however not to tear the tissue or leave any pigmented spot behind or expose the bone. Next, a straight fissure no. 8 diamond bur mounted on contra-angled handpiece was used (Figure 5) again with copious lavage. It is recommended to use the appropriately larger size bur for abrasion. The smaller ones do not only smoothen surface easily, but also have a tendency to make small pits in the area which needs subsequent correction. In this case, the feather-light brushing strokes were made use of to attain goal of completely eliminating the remnants (Figure 6), without holding the bur at one place only. Lastly, depending on the extent of the manoeuvre, the thus denuded lamina propria was shielded with COE PAK™ (Figure 7) intended to be in place for a week.
DISCUSSION
Oral pigmentation occurs in all races of man still the intensity and distribution of in oral mucosa is variable; not only between races but also between different individuals of the same race and again within different areas of the same mouth [4]. The degree of pigmentation is partially related to mechanical, chemical, and physical stimulation [10]. Melanin pigmentation as in our case is frequently caused by melanin deposition by active melanocytes located mainly in the basal and suprabasal layer of the oral epithelium.
For the reason that patient gave a history of allergy to lignocaine injection, that atricaine was administered. Moreover, comparing articaine to the routine lignocaine, the potency of articaine is believed to be 1.5 times to that of lignocaine and its toxicity is 0.6 to that of lignocaine [11]. So even a lesser equivalent of former predictably numbs the area adequately. We adopted a stereotypical approach to address the issue although there is an evidence of various other above-mentioned ways used earlier. The gingival biotype, clinician’s expertise, patient preferences, and recurrence rate, greatly determine the selection of a technique. A recent research utilized plasma as a novel treatment technique for gingival hyperpigmentation and gummy smile [3]. Plasma is the fourth state of matter and the mechanism is based on the release of ozone, the free radicals and reactive species.
An uneventful healing was observed with absence of postoperative pain, haemorrhage, infection or scarring (Figure 8) on first follow-up visit. A critical concern in the management is a high rate of relapse. Repigmentation refers to the clinical appearance of melanin pigment following a period of clinical depigmentation [3]. The complete removal of remnants could possibly explain the fact that there was no repigmentation (Figure 9) at three months interval. The patient is further monitored for the same. There is paucity of data and majority of the available literature so far is comprised of case reports. The need of the hour is randomized controlled longitudinal studies to identify the efficiency and effectiveness of available solutions.
CONCLUSION
Patient’s acceptance of the attempt was good and results were excellent as perceived by the patient. Growing cosmetic demands for gum sculpting and relieving gum discoloration necessitates any dental set-up to be fully equipped with lasers and other modern devices. Having said that, it is equally expected from a dental professional to have a sound knowledge, as well as expertise in conventional knacks.
ACKNOWLEDGEMENTS
None.
CONFLICTS OF INTEREST
Nil.
DECLARATION OF PATIENT’S CONSENT
The authors certify that they have obtained an appropriate patient consent form. In the form the patient/ parents’ have given their consent for the images and other clinical information to be reported in the journal. The patient understands that the names and initials will not be published and due efforts will be made to conceal the identity, but anonymity cannot be guaranteed.
REFERENCES
- Asopa V. (2013). Management of adverse tissue response to faulty pontic design – A case report. Int J Prosthet Dent. 4:26-30.
- Lombardi RE. (1973). The principles of visual perception and their clinical application to denture esthetics. J Prosthet Dent. 29:358-382.
- Alasmari DS. (2018). An insight into gingival depigmentation techniques. The pros and cons. Int J Health Sci (Qassim). 12:84-89.
- Wagle SV, Agrawal AA, Sankhe R. (2018). Gingival depigmentation using scalpel. Biomed Biotechnol Res J. 2:223-225.
- Malhotra S, Sharma N, Basavaraj P. (2014). Gingival esthetics by depigmentation. J Periodontal Med Clin Pract. 1:79–84.
- Dummett CO, Bolden TE. (1963). Post-surgical clinical repigmentation of the gingiva. Oral Surg Oral Med Oral Pathol. 16:353–365.
- Kumar S, Bhat GS, Bhat KM. (2013). Comparative evaluation of gingival depigmentation using tetrafluoroethane cryosurgery and gingival abrasion technique:Two years follow up. J Clin Diag Res. 7:389–94.
- Mahesh HV, Harish MR, Shashikumar BM, Ramya KS. (2012). Gingival pigmentation reduction:A novel therapeutic modality. J Cutan Aesthet Surg. 5:137–140.
- Atsawasuwan P, Greethong K, Nimmanon V. (2007). Treatment of gingival hyperpigmentation for esthetic purposes by ND:YAG laser: Report of 4 cases. J Periodontol. 71:315–321.
- Ciçek Y, Ertaş U. (2003). The normal and pathological pigmentation of oralmucous membrane: A review. J Contemp Dent Pract. 4:76‑86.
- Bansal SK, Kaura S, Sangha PK, Kaur P, Bahl R, et al. (2018). Comparison of anesthetic efficacy of 4% articaine versus 2% lignocaine. Indian J Dent Sci. 10.
Copyright: Munjal S, et al. (2020). This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Citation: Munjal S, et al. (2020). Demystifying the Depigmentation Manoeuvre: A Pragmatic Approach. Dental. 2(1):05.
 Abstract
Abstract  PDF
PDF